
5 Steps to Restore the Core!
Chris Kelly CSCS (NSCA), CES, PES (NASM)
This information is from Chris Kelly’s eLearning continuing education course:
Restore the Core: Integrated Core Training for Real World Function. See the full course for additional core assessments with video, and several core exercises and progressions with videos.
Part 2 of the Core Series is Core Complete Training: A Systematic Approach for Aesthetic Core Development by Chris Kelly.
Five Step Process for Restoring the Core
Much like a weight belt, the abdominals tighten around the spine to provide support during exercise or daily tasks such as bending over and rotating. Contracting the abs in this fashion is known as an abdominal brace.
While this reaction happens automatically with healthy adults, a lack of conscious control or a poor understanding of how to do it during exercise is often related to a host of issues such as back pain and weakness of core muscles deep inside the body.
While the outer core consists of the visible stomach muscles (rectus abdominis, internal and external obliques), the muscles of the inner core are located close to our joints (multifidus, diaphragm, pelvic floor and transversus abdominis). Although these muscles are too weak to actually move the limbs, their function is to contract isometrically before movement occurs to stabilize the joints.
The most important thing to understand about this idea is that these muscles must fire before any movement takes place to allow stability to occur. Interestingly, a timing delay in this reaction has been found to exist in clients with chronic back pain illustrating the fact that the presence of chronic or acute pain can throw off the way the inner core fires and stabilizes the body.
By contrast, the muscles of the outer core are responsible for moving or preventing motion of the extremities and trunk after the inner core muscles have fired. A common error made in training programs for clients who are de-conditioned or returning from injury is an overabundance of outer core training without re-establishing control of the inner core muscles. The first step in a progressive core training program is to establish the status of the muscles of the inner core as well as whether the client possesses conscious abdominal control.
This is accomplished via assessments as well as subjective observation. Once the need for this type of training has been established, the goal of the program becomes bringing these muscles back to function while teaching conscious control of the abdominals.
We use a simple five step process for restoring the core to increase function for abdominal training as well as daily life.
Step 1: Regain Mobility
One of the more important concepts in fitness and/or rehabilitation is mobility before stability. If a joint does not possess the ability to move correctly, it can only stabilize through its limited range of motion. With this in mind, the first order of business is to get your client to stretch and use the foam roll for the following muscles:
- Psoas and Quadriceps
- Gluteus Medius and Gluteus Maximus
- Latissimus Dorsi
- Hip Abductors and Adductors
These muscles directly act upon the pelvis and are often tight and restricted.
In creating the mobility program for a client, consider the following:
- Identify the basic purpose of myofascial release (foam rolling.)
- Determine the number of rolls per muscle the client should perform on each area.
- Determine the primary areas targeted for foam rolling and stretching.
- Identify the order of foam rolling, stretching and hip mobility in the warm up process.
Sample Video of Mobility
Step 2: Breathe and Brace
After foam rolling and stretching, the session continues with a simple drill to teach the client to re-establish deep breathing. This exercise can be seen as a “bang for your buck” movement because we are training the diaphragm while relieving stress and tension getting the client into the right frame of mind to exercise.
This drill can be performed by asking the client to inhale deeply through the nose while expanding the stomach, hold the breath for a slow three count and release through the mouth. At the same time, watch the position of the chest to ensure it is not rising.
While it will likely take several sessions for the client to gain an understanding of this method of breathing, practicing this drill both in your warm up and as homework will improve conscious control of this breathing pattern until it becomes unconscious habit.
Once the client has gained a working understanding of breathing, the next concept is to re-establish conscious abdominal control. This can be done by teaching them to actively “brace” or contract their abs. A brace involves tightening the abs as if to avoid being poked in the stomach.
This drill can be practiced by placing one hand on the stomach and one hand slightly above the small of the low back. Apply pressure by pushing into the stomach while tightening your abs to resist. You will feel your back extensor and abdominal muscles simultaneously tighten. Beginners should hold each brace for 5-10 seconds and then release several times to become familiar with this action. As this becomes easier, the length of each hold increases while the client breathes normally.
The ultimate goal of bracing is to consciously tighten the abs to stabilize the trunk against movement of the extremities. While bracing only requires around a 20% abdominal contraction for daily life activities, these demands are greatly increased during tasks which require increased stability such as resistance training or sports. The trick is to “tune” the brace by allowing contracting as much as necessary in given situations.
With this in mind, the final bracing progression incorporates leg movement while breathing and bracing normally.
Sample Video of Abdominal Bracing
Step 3: Mobilize the Hips
In looking at the body as an integrated unit, consider that certain joints are built to move while others require stability. While the goal of bracing is to tone the muscles around the spine to decrease or prevent motion of the torso, we want to gain movement at the hips (the joints directly above and below the lumbar spine) and thoracic spine to allow normal movement to occur. This task can be accomplished through mobility drills for the hips and thoracic spine while maintaining an abdominal brace in various standing positions.
Because new clients often lack knowledge of coordinated movements, the phase one series begins against a wall. Pressing in to the wall allows the client to balance while pressing in to the wall to maintain abdominal bracing and normal breathing.
Exercises in this phase are simple in nature and intended to mobilize the hips and t-spine in multiple planes of motion. As the client gains proficiency in both bracing and movement, move off the wall for phase two progression by engaging in more complex and integrated movements. For each phase, perform each drill back to back once for 10 reps or 20-30 seconds each.
Sample Video of Hip Mobilization
Step 4: Free Standing Strength Training
Though weight lifting is traditionally viewed as an opportunity to strengthen the limbs, the truth is that any free standing exercise can also be seen as core training by simply initiating an abdominal brace during the activity. Certain exercises can be modified to increase the stabilization requirements in specific directions.
These include:
Anti-rotation Exercises:
Exercises which involve pressing, pulling or carrying weight on one side of the body forcing muscles of the core to prevent rotation or lateral flexion of the torso.
Anti-extension Exercises:
Exercises which involve pressing overhead, rowing against gravity or pushing up against gravity forcing the core to prevent excess extension of the torso or arching of the back.
Including these exercises in your training program allows you to mimic situations for your client which increase stability demands such as carrying a briefcase and lifting items overhead.
Sample Video of Standing Strength Training Exercise
Step 5: Progress Your Planks
After the re-establishment of breathing patterns and the ability to actively brace the abdominals in supine position (lying on the back), progress to more advanced exercises such as planks.
The key to a plank is to first find a neutral spine position while remaining on all fours. From there, raise into a plank position while maintaining the brace and neutral spine position. A dowel rod or broom stick can be placed on the client’s back to teach the back to stay in position while the stomach can be poked at various angles to ensure the client is maintaining the abdominal brace.
Beginning as a static hold, the plank is utilized to build isometric endurance while teaching the torso to resist movement. Once this exercise can be held statically for time, it can be progressed by moving the arms and legs while maintaining a stable torso.
Sample Video of Plank Progressions
About the Author
Chris Kelly is an experienced fitness journalist, speaker, and strength coach. With over ten years in the fitness industry, Chris’s experience spans from work in rehabilitation settings to strength and conditioning for athletes.
As a fitness speaker, Chris has authored numerous seminars and workshops focusing on back pain and restorative core training along with a variety of related topics. He holds fitness certifications from the National Academy of Sports Medicine and the National Strength and Conditioning Association. Chris received a bachelor’s degree in communications from St. Johns University in Queens, New York, and a master’s degree in journalism with a specialization in health and science from Columbia University in New York City.
An experienced health writer, Chris has also written extensively on fitness, healthcare, and nutrition. His writing has appeared in numerous publications including Exercise for Men, Prevention, Health, and the Boston Globe





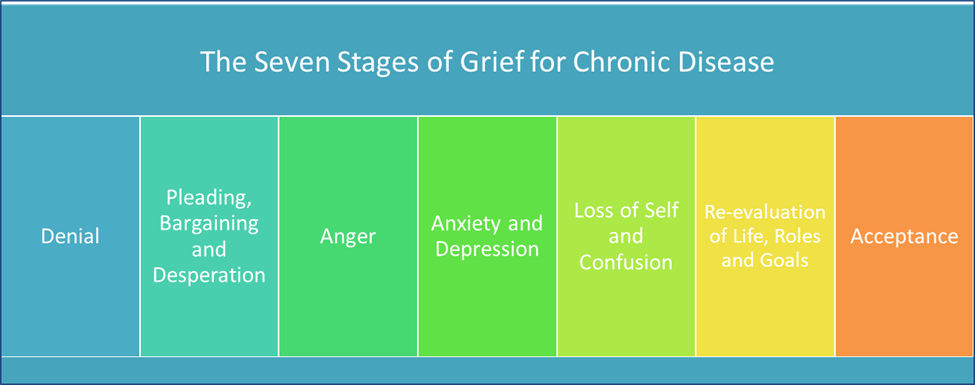





 Exercise is an important part of treatment. Research shows that it may help slow the progression of disease. Be patient and creative when working with clients who have Alzheimer’s disease. Have an understanding of the disease progression, be vigilant in identifying physical decline, and overall, adjust their exercise program to maintain safety. The seven stage model that is commonly accepted and used to stage the progression of Alzheimer’s is provided below.
Exercise is an important part of treatment. Research shows that it may help slow the progression of disease. Be patient and creative when working with clients who have Alzheimer’s disease. Have an understanding of the disease progression, be vigilant in identifying physical decline, and overall, adjust their exercise program to maintain safety. The seven stage model that is commonly accepted and used to stage the progression of Alzheimer’s is provided below.